The Science
Health Screening NZ, in partnership with CardiAction, is dedicated to delivering accessible, science-driven healthcare solutions. CardiAction’s use of advanced Pulse Wave Analysis (PWA) technology is based on robust cardiovascular research, enabling assessment of heart health with precision.
Guided by the latest findings in cardiovascular science, we continually update our screening technology, refine report data, and enhance aftercare recommendations to ensure the highest standard of care. Our commitment to evidence-based innovation means each CardiAction screening empowers clients with accurate, actionable insights into their cardiovascular health.
If you are a doctor looking for more information about CardiAction, visit the Doctor FAQ’s.
Equipment
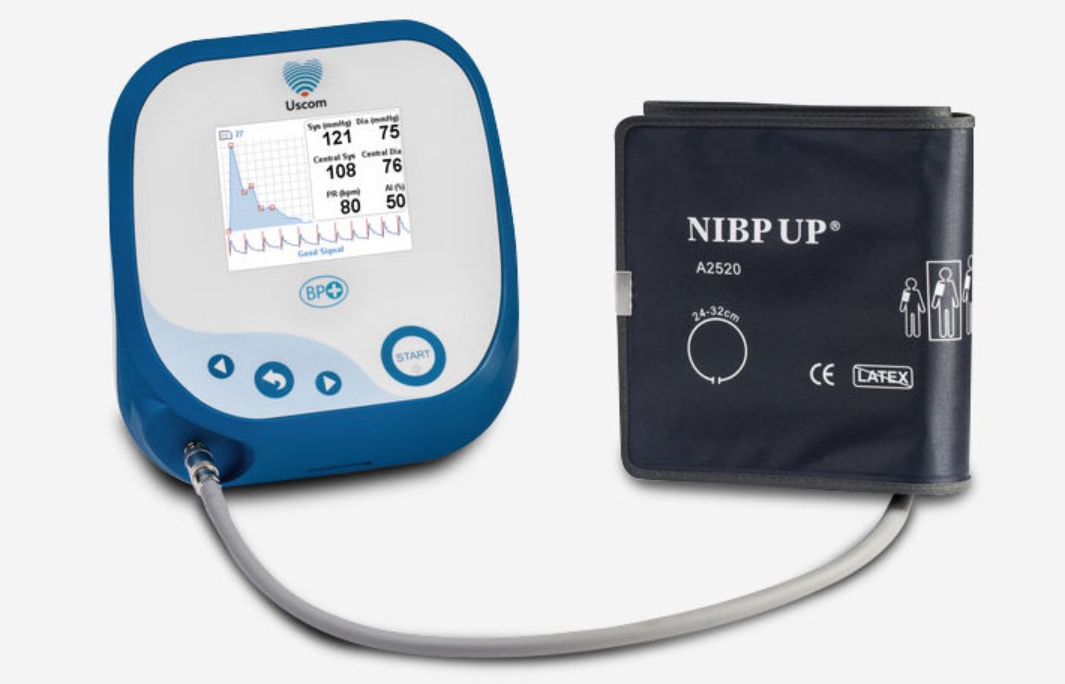
Health Screening NZ uses the Uscom BP+ which has been developed to revolutionise hypertensive care. This PWA is FDA and TGA approved and is used by a variety of different health care professionals including in research and general practice.
Uscom maintains a reference of all current evidence for the BP+ product. Some of this key evidence can be seen here:
Health Screening NZ utilises the Uscom BP+ device, a revolutionary tool in hypertensive care and cardiovascular risk assessment. This Pulse Wave Analysis (PWA) device is FDA and TGA approved, and is widely trusted by healthcare professionals in both clinical research and general practice settings. The Uscom BP+ allows us to provide accurate, non-invasive cardiovascular screenings as part of our CardiAction service.
For more detailed information on the scientific validation and educational resources behind the Uscom BP+, please visit:
Research Behind CardiAction
CardiAction has been developed through rigorous research and refinement over the past 10 years, led by the 3p Healthcare Scientific Director, Dr Paul Beaver, in collaboration with Dr John Cook, who serves as Medical Advisor to Health Screening NZ. This extensive research has shaped CardiAction’s capabilities, allowing us to offer a precise, evidence-based approach to cardiovascular screening. Below, Dr Beaver provides a summary of key studies that support the science behind CardiAction.
Summary of Central Aortic Pulse Wave Analysis Research
BACKGROUND
Cardiovascular disease encompasses many different conditions, such as heart attacks (Myocardial Infarctions MI), stroke and blood vessel diseases, such as atherosclerosis. High blood pressure—also known as hypertension—is responsible for more deaths and disease worldwide than any other single health risk factor (Lim et al, 2012). High blood pressure is a major risk factor for chronic diseases including stroke, coronary heart disease CHD, heart failure and chronic kidney disease CKD (National Heart Foundation of Australia, 2015).
The traditional approach used for the evaluation, prevention, and treatment of cardiovascular diseases (CVD) and coronary heart diseases (CHD), is to use the top 5 cardiovascular risk factors, that are:
- Hypertension
- Dyslipidaemia (elevated total or low-density lipoprotein (LDL) cholesterol levels diabetes
- Impaired glucose tolerance
- Smoking
- Obesity
Unfortunately, this approach seems to have reached its limit as it can only identify approximately 50% of people, based on having the 5 risk factors within the so-called ‘normal’ range, who will continue to have CHD (Houston, 2012). This is referred to as the ‘CHD gap’ (Houston, 2010).The stiffness of our arteries is now recognised as a major risk factor for cardiovascular health diseases, such as hypertension (Vlachopoulos et al, 2010).
Over the past two decades, new cardiovascular research, technological advancements, such as central aortic Pulse Wave Analysis (PWA) plus new blood pressure data and assessment concepts have highlighted the importance of central aortic(c-BP) above and beyond the existing clinical value of the traditionally measured brachial BP. The European Society of Hypertension/European Society of Cardiology guidelines for the management of arterial hypertension suggested the measurement of aortic pulse wave velocity (PWV), which is considered the gold standard method for assessing aortic stiffness, as a tool for assessment of subclinical target organ damage (Mancia et al, 2007) for early detection, and aggressive prevention and treat CVD before clinical events occur [Houston, 2012).
SELECTED REFERENCES
- Houston MC. Nutrition and nutraceutical supplements in the treatment of hypertension. Expert Rev Cardiovasc Ther., (2010), 8: 821-833.
- Houston MC. What Your Doctor May Not Tell You About Heart Disease. (2012). Grand Central Life and Style. Hachette Book Group. (2012). 237 Park Ave. New York, USA.
- Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H et al. A comparative riskassessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet, 380:2224–60.
- Mancia G, De Backer G, Dominiczak A, et al. guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2007; 25:1105–87.
ACCURACY OF PWA DEVICES
The non-invasive estimation of c-BP is achieved by several techniques of varying complexity, and using different mathematical transfer functions (each with various assumptions) or modes of calibration, for example. see some the selected references below.
A systematic review and meta-analysis of 22 eligible studies of 808 study participants, which validated estimating central aortic-SBP non-invasively, using different commercial Pulse Wave Analysis devices, by comparing results against BP measurements from invasive Catheter type testing, was undertaken to determine the accuracy of commercial devices estimating central aortic-SBP non-invasively. The estimated (non-invasive) aortic-SBP differed from the actual (invasive) value by -1.08mmHg (95%CI: -2.81, 0.65 mmHg) when invasive Catheter type measurements of BP values were used. (Papaioannou et al, 2016, see below). The meta-analysis concluded that overall, the estimation of c-SBP by the available devices is very accurate, but only when the devices are calibrated using invasive intra-arterial BP measurements.
Furthermore suprasystolic oscillometry PWA has been shown to: (1) yield central systolic BPs that are highly correlated with those assessed by catheter measurement at the ascending aorta or aortic arch(Lin et al, 2012) and, (2) measure central systolic BP with good intra-test and inter-test reliability (intraclass correlation coefficients=0.975 and 0.895, respectively)(Climie et al, 2012).
SELECTED REFERENCES
- Climie RED, Schultz MG, Nikolic SB, Ahuja KDK, Fell JW, Sharman JE. Validity and reliability of central blood pressure estimated by upper arm oscillometric cuff pressure. Am J Hypertens 2012; 25: 414–420.
- Costello BT, Schultz MG, Black JA, Sharman JE. Evaluation of a brachial cuff and suprasystolic waveform algorithm method to noninvasively derive central blood pressure. American Journal of Hypertension. 2015 Apr 1;28(4):480-6.
- Lin AC, Lowe A, Sidhu K, Harrison W, Ruygrok P, Stewart R. Evaluation of a novel sphygmomanometer, which estimates central aortic blood pressure from analysis of brachial artery suprasystolic pressure waves. J Hypertens 2012;30: 1743–1750.
- Lowe A, Harrison W, El-Aklouk E, Ruygrok P, Al-Jumaily AM. Noninvasive model-based estimation of aortic pulse pressure using suprasystolic brachial pressure waveforms. J Biomech 2009;42: 2111–2115.
- Papaioannou TG, Karageorgopoulou TD, Sergentanis TN, Protogerou AD, Psaltopoulou T, Sharman JE, Weber T, Blacher J, Daskalopoulou SS, Wassertheurer S, Khir AW. Accuracy of commercial devices and methods for noninvasive estimation of aortic systolic blood pressure a systematic review and meta-analysis of invasive validation studies. Journal of hypertension. 2016 Jul 1;34(7):1237-48.
- Park CM, Korolkova O, Davies JE, Parker KH, Siggers JH, March K, Tillin T, Chaturvedi N, Hughes AD. Arterial pressure: Agreement between a brachial cuff-based device and radial tonometry. J Hypertens 2014;32: 865–872.
- Sharman JE, Avolio AP, Baulmann J, Benetos A, Blacher J, Blizzard CL, Boutouyrie P, Chen CH, Chowienczyk P, Cockcroft JR, Cruickshank JK. Validation of non-invasive central blood pressure devices: ARTERY Society task force consensus statement on protocol standardization. European heart journal. 2017 Oct 1;38(37):2805-12.
- Sluyter JD, Camargo Jr CA, Scragg RK. Ten-second central SBP variability predicts first and recurrent cardiovascular events. Journal of hypertension. 2019 Mar 1;37(3):530-7.